Are you a good candidate for VBAC?
This blog post is intended to provide additional information apart from what we have mentioned in our video with the title “are you a good candidate for VBAC?” Moreover, on this page, you can find the entire list of scientific research studies which this video is based on.
In our video, we discuss the 14 factors which determine whether or not you are a good candidate for VBAC. Please watch it first, so that you understand the information that we mention below the video!
Type of Uterine Incision
If you check out the following research study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7396476/ you will find an illustration of the different kinds of uterine incisions which the medical team may have used in your case (figure 1). As mentioned in the video, a low transverse (= low horizontal) incision is the best incision for a VBAC. Moreover, a high vertical incision (= classical incision) significantly increases the risk of uterine ruptures which is why it is normally not recommended to try having a VBAC in such a case. In all other cases which you can see in the illustration, the level of risk involved is not so clear because there is not enough scientific research. Because of that, it is recommended to discuss the pros and cons with your doctor based on your particular case.
Uterine Scar Thickness
Unfortunately, answering the question “what is a good uterine scar thickness?” is very difficult because at this point more research is needed. However, most researchers concluded that a uterine scar thickness of at least 3.0mm – 3.5mm comes with a low risk of uterine rupture IF you had a low horizontal incision (unfortunately, most research on scar thickness only focuses on low horizonal incisions only which is why we don’t know what a good scar thickness for other types of incisions is). That said, it does not mean that you cannot have a VBAC if your scar thickness is less than 3.0-3.5mm. However, the risk of uterine rupture increases.
BISHOP Score
The BISHOP score is defined by the following 5 factors:
- Consistency of the cervix (the softer, the higher the score)
- Effacement of the cervix (the more it has thinned out, the higher the score)
- Dilation of the cervix (the more dilated, the higher the score)
- Position of the cervix (the more “anterior” (nearer to the vagina), the higher the score)
- Fetal Station (the further the baby has descended, the higher the score)
The maximum Bishop score is 13, as a woman may receive 3 points at most for each one of the first three criteria and 2 points at most for the remaining two criteria.
A score equal to or above 8 is associated with increased chances that the woman goes into labor spontaneously and/or that labor induction is going to be success.
Based on these factors, it is obvious why a higher score is more desirable: the higher the score, the more likely it is that a woman goes into labor spontaneously.
There are several ways to increase your BISHOP SCORE and to increase your chances of going into labor spontaneously:
Help your body prepare your cervix for labor from week 37 onwards, with the tools that we explain in this video: https://youtu.be/8rehbupwhzY
Try exercises on a birthing ball which we explain in this video: https://youtu.be/UgrbOc4cebY
Baby Weight
When it comes to the “optimal” baby’s weight for a vaginal birth, please note that it is not only about the baby’s weight. It’s also about the size of your pelvis and the question, how easily your baby can move through your pelvis – given the size of your baby.
While a fetal weight of more than 4000 grams is considered a lot, keep in mind that there are women who have given birth to babies whose weight was closer to 5000 grams – and even higher. So, it really depends on your particular case, how much fetal weight is considered too much.
Sources which our Video is based on
Basic E, Basic-Cetkovic V, Kozaric H, Rama A. Ultrasound evaluation of uterine scar after cesarean section. Acta Inform Med. 2012 Sep;20(3):149-53. doi: 10.5455/aim.2012.20.149-153. PMID: 23322970; PMCID: PMC3508848. https://pubmed.ncbi.nlm.nih.gov/23322970/
Basic E, Basic-Cetkovic V, Kozaric H, Rama A. Ultrasound evaluation of uterine scar after Cesarean section and next birth. Med Arch. 2012;66(3 Suppl 1):41-4. doi: 10.5455/medarh.2012.66.s41-s44. PMID: 22937691. https://pubmed.ncbi.nlm.nih.gov/22937691/
Bujold E, Hammoud A, Schild C, Krapp M, Baumann P. The role of maternal body mass index in outcomes of vaginal births after cesarean. Am J Obstet Gynecol. 2005 Oct;193(4):1517-21. doi: 10.1016/j.ajog.2005.03.041. PMID: 16202749. https://pubmed.ncbi.nlm.nih.gov/16202749/
Cahill AG, Tuuli M, Odibo AO, Stamilio DM, Macones GA. Vaginal birth after caesarean for women with three or more prior caesareans: assessing safety and success. BJOG. 2010 Mar;117(4):422-7. doi: 10.1111/j.1471-0528.2010.02498.x. Epub 2010 Jan 28. PMID: 20374579. https://pubmed.ncbi.nlm.nih.gov/20374579/
Calì G, Timor-Tritsch IE, Palacios-Jaraquemada J, Monteaugudo A, Buca D, Forlani F, Familiari A, Scambia G, Acharya G, D’Antonio F. Outcome of Cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018 Feb;51(2):169-175. doi: 10.1002/uog.17568. PMID: 28661021. https://pubmed.ncbi.nlm.nih.gov/28661021/
Durnwald CP, Ehrenberg HM, Mercer BM. The impact of maternal obesity and weight gain on vaginal birth after cesarean section success. Am J Obstet Gynecol. 2004 Sep;191(3):954-7. doi: 10.1016/j.ajog.2004.05.051. PMID: 15467571. https://pubmed.ncbi.nlm.nih.gov/15467571/
Fox NS, Namath AG, Ali M, Naqvi M, Gupta S, Rebarber A. Vaginal birth after a cesarean delivery for arrest of descent. J Matern Fetal Neonatal Med. 2019 Aug;32(16):2638-2642. doi: 10.1080/14767058.2018.1443069. Epub 2018 Feb 27. PMID: 29455594. https://pubmed.ncbi.nlm.nih.gov/29455594/
Gulersen, Moti MD, MSC; Grunebaum, Amos MD; Bornstein, Eran MD; Chervenak, Frank MD Inter-delivery Time Interval and the Likelihood of Successful Vaginal Birth After Cesarean Delivery. Obstetrics & Gynecology: May 2020 – Volume 135 – Issue – p 172S-173S. doi: 10.1097/01.AOG.0000663892.02700.9b. https://journals.lww.com/greenjournal/Abstract/2020/05001/Inter_delivery_Time_Interval_and_the_Likelihood_of.612.aspx
Guise JM, Eden K, Emeis C, Denman MA, Marshall N, Fu RR, Janik R, Nygren P, Walker M, McDonagh M. Vaginal birth after cesarean: new insights. Evid Rep Technol Assess (Full Rep). 2010 Mar;(191):1-397. PMID: 20629481; PMCID: PMC4781304. https://pubmed.ncbi.nlm.nih.gov/20629481/
Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. 2005 Oct;106(4):741-6. doi: 10.1097/01.AOG.0000177972.32941.65. PMID: 16199630. https://pubmed.ncbi.nlm.nih.gov/16199630/
Kessous R, Sheiner E. Is there an association between short interval from previous cesarean section and adverse obstetric and perinatal outcome? J Matern Fetal Neonatal Med. 2013 Jul;26(10):1003-6. doi: 10.3109/14767058.2013.765854. Epub 2013 Feb 14. PMID: 23311913. https://pubmed.ncbi.nlm.nih.gov/23311913/
Mei JY, Havard AL, Mularz AJ, Maykin MM, Gaw SL. Impact of Gestational Weight Gain on Trial of Labor after Cesarean Success. Am J Perinatol. 2019 Aug;36(10):1023-1030. doi: 10.1055/s-0038-1675624. Epub 2018 Nov 30. PMID: 30500964. https://pubmed.ncbi.nlm.nih.gov/30500964/
Qu ZQ, Yang MH, Du MY, Ma C, Tao YP, Chen Z, Liang K, Ma RM. [Outcome of vaginal birth after cesarean section in women with advanced maternal age]. Zhonghua Fu Chan Ke Za Zhi. 2017 Aug 25;52(8):521-525. Chinese. doi: 10.3760/cma.j.issn.0529-567X.2017.08.004. PMID: 28851168. https://pubmed.ncbi.nlm.nih.gov/28851168/
Royal College of Obstetricians and Gynecologists: Birth After Previous Caesarean Birth. Green-top Guideline No. 45. October 2015. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_45.pdf
Shinar S, Agrawal S, Hasan H, Berger H. Trial of labor versus elective repeat cesarean delivery in twin pregnancies after a previous cesarean delivery-A systematic review and meta-analysis. Birth. 2019 Dec;46(4):550-559. doi: 10.1111/birt.12434. Epub 2019 May 23. PMID: 31124186. https://pubmed.ncbi.nlm.nih.gov/31124186/
Srinivas SK, Stamilio DM, Sammel MD, Stevens EJ, Peipert JF, Odibo AO, Macones GA. Vaginal birth after caesarean delivery: does maternal age affect safety and success? Paediatr Perinat Epidemiol. 2007 Mar;21(2):114-20. doi: 10.1111/j.1365-3016.2007.00794.x. PMID: 17302640. https://pubmed.ncbi.nlm.nih.gov/17302640/
Spaans WA, van der Vliet LM, Röell-Schorer EA, Bleker OP, van Roosmalen J. Trial of labour after two or three previous caesarean sections. Eur J Obstet Gynecol Reprod Biol. 2003 Sep 10;110(1):16-9. doi: 10.1016/s0301-2115(03)00082-4. PMID: 12932864. https://pubmed.ncbi.nlm.nih.gov/12932864/
Srinivas SK, Stamilio DM, Sammel MD, Stevens EJ, Peipert JF, Odibo AO, Macones GA. Vaginal birth after caesarean delivery: does maternal age affect safety and success? Paediatr Perinat Epidemiol. 2007 Mar;21(2):114-20. doi: 10.1111/j.1365-3016.2007.00794.x. PMID: 17302640. https://pubmed.ncbi.nlm.nih.gov/17302640/
Tahseen S, Griffiths M. Vaginal birth after two caesarean sections (VBAC-2)-a systematic review with meta-analysis of success rate and adverse outcomes of VBAC-2 versus VBAC-1 and repeat (third) caesarean sections. BJOG. 2010 Jan;117(1):5-19. doi: 10.1111/j.1471-0528.2009.02351.x. PMID: 19781046. https://pubmed.ncbi.nlm.nih.gov/19781046/
Tanos V, Toney ZA. Uterine scar rupture – Prediction, prevention, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2019 Aug;59:115-131. doi: 10.1016/j.bpobgyn.2019.01.009. Epub 2019 Feb 10. PMID: 30837118. https://pubmed.ncbi.nlm.nih.gov/30837118/
Trojano G, Damiani GR, Olivieri C, Villa M, Malvasi A, Alfonso R, Loverro M, Cicinelli E. VBAC: antenatal predictors of success. Acta Biomed. 2019 Sep 6;90(3):300-309. doi: 10.23750/abm.v90i3.7623. PMID: 31580319; PMCID: PMC7233729. https://pubmed.ncbi.nlm.nih.gov/31580319/
Wu Y, Kataria Y, Wang Z, Ming WK, Ellervik C. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019 Oct 17;19(1):360. doi: 10.1186/s12884-019-2517-y. PMID: 31623587; PMCID: PMC6798397. https://pubmed.ncbi.nlm.nih.gov/31623587/
Medical Disclaimer: The information on this page is not intended to diagnose, prevent, mitigate, treat or cure any disease! It is not personal medical advice. We recommend that you ask a doctor whenver you are looking for medical advice!
ABOUT THE AUTHORS
Nathalie Kaufmann & Mathias Ritter
Nathalie is a pregnancy and birth Consultant and a TCM Therapist with almost 20 years of experience in Traditional Chinese Medicine (TCM), acupuncture, reflexology, Shonishin baby massage techniques, Western and Eastern massage techniques (including TUINA), as well as herbal medicine and nutrition.
She has worked in hospitals across London and was Head of the Maternity Acupuncture Clinic at the Whittington hospital in London. Today, Nathalie runs her own practice in London and helps pregnant women with pregnancy- and birth-related issues. She also specializes in alternative treatments for babies and children.
Mathias is a Researcher and Science Geek who holds two Master of Science degrees. He has been involved in several health-related businesses over the past 10 years and has held presentations about health-related topics across Europe. He specializes in research regarding pregnancy-, birth and baby-related topics.
RELATED POSTS
How to increase the Oxygen Supply to the Baby in the Womb
During your pregnancy, there is a constant supply of oxygen to your baby. But what pregnant women often don’t know is that there are certain things that can reduce the oxygen supply to the baby. Luckily though, there are also very simple ways to increase the oxygen...
Best sitting Position to help Baby find a good Position in the Womb
As they approach the end of their pregnancy, many moms-to-be start to worry. How should they help baby find a good position for labor? What about turning baby head down? What if baby is posterior? And how should I help baby engage in my pelvis?So, how can you help...
Pregnancy Vitamins: What Nutrients does a Fetus need & what Foods should I eat?
This blog post adds to our video on youtube in which we go through our list of the 9 most important micronutrients every fetus needs. If you have not watched our video so far, we recommend doing that first:Below, you can find a list of all the nutrients that we...
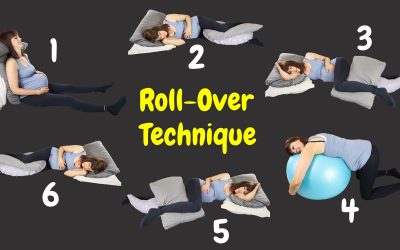
How to keep moving with an epidural
This blog posts adds to the video "8 reasons why labor can stall and what to do about it". In that video, among others, we explain the "roll-over technique from Penny Simkin (see sources below) which allows a woman to keep moving even when she is confined to bed....
How to keep track of Baby’s Movements
If your baby is active in your womb, then it is a sign that your baby is well. Because of that, most doctors recommend counting your baby's kicks from week 28 of your pregnancy onwards. In this brief blog post, we want to explain how you can keep track of your baby's...
How to relieve Pelvic Girdle Pain during Pregnancy
This blog post complements the information from our video on youtube on how to relieve pelvic girdle pain during pregnancy. In that video, we propose 2 ways to relieve pelvic girdle pain: 1. some minor changes in your lifestyle and 2. exercises. While the video...
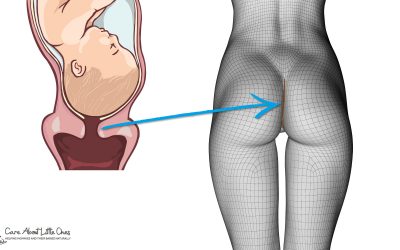
The Purple Line – Find Out If You Are Dilating
The purple line can tell a woman if and how much she is dilated. So in this blogpost, we explain how to find out if you are dilating and how much you are approximately dilated.
How Effective Is Reflexology to Induce Labor?
Many women in their late pregnancy hope that reflexology can help them induce labor naturally. And indeed, reflexology is ONE of the tools that I apply to help women go into labor.So, how effective is reflexology to induce labor? Reflexology could help you induce...
Best Sleeping Position To Turn A Breech Baby (with Pictures)
Most babies turn at night. But unfortunately, not every sleeping position provides the baby with enough room to turn. As a result, many babies remain in a breech presentation. Luckily though, sleeping in the right position can support baby turn head down.So, what is...
LEAVE A REPLY







0 Comments